Veins are blood vessels that help bring blood back to the heart. The increased pressure in the superficial veins can lead to the development of varicose veins.
Varicose veins can develop anywhere on the body, but the lower extremities are most commonly affected.
Many factors can increase the risk of developing varicose veins, including:
- inheritance
- excess weight
- old age
- pregnancy
- work that requires prolonged sitting or standing
Varicose veins can be treated with non-invasive methods, with little time and without changing the usual rhythm of life. The main goal of treatment is to relieve symptoms, prevent complications and achieve good cosmetic results. Varicose veins are enlarged, can be deformed and cause pain. They are usually raised above the skin and convex and also have a red or bluish color.
Varicose veins often occur through an underlying condition known as chronic venous insufficiency. Varicose veins are very common, especially in women.
Predisposition to varicose veins
Varicose veins can occur in men or women of any age. Most often it occurs:
- women who have had multiple pregnancies
- in postmenopausal women
- in men over the age of 50
- in people of any age who have varicose veins in the family
- in men and women with jobs that require prolonged sitting or standing, such as nurses, teachers, drivers, etc.
What are the causes of varicose veins?
Varicose veins usually develop in the legs because the veins in the legs have to pump blood to the heart against gravity.
Less common causes of varicose veins are phlebitis (inflammation of the veins) and congenital anomalies of the veins. Varicose veins are usually caused by a condition called venous insufficiency.
- Venous valves. The veins in the legs have valves that prevent the backflow of blood. When the functioning of these valves is disturbed, the blood in the veins begins to accumulate and is not fully delivered to the heart.
- Dilated veins. The veins widen and the increased pressure leads to the development of varicose veins.
- Weakness of the walls of the veins. Additionally, weakness of the vein walls (due to trauma or blood clots in the past) can also lead to valve damage and the formation of varicose veins.
What are the symptoms of varicose veins?
Many cases of varicose veins are asymptomatic, but visual signs of venous involvement include:
- Wide, tortuous and protruding veins
- Swollen ankles, sore feet
- Feeling of heaviness in the legs, especially at night
- Telangiectasia (spider veins) in the same area as varicose veins
- Lipodermatosclerosis (hard fatty deposits under the skin)
- Change the skin color to bluish or brown on the shins and ankles
- Varicose eczema (congestive dermatitis) dry, itchy, red skin in the affected area
- leg cramps
- restless legs syndrome
How to cure varicose veins?
There are various types of treatment for varicose veins. The best treatment will depend on the structure of your venous system:
- Location and size of the affected vein
- Presence or absence of symptoms
- Presence of associated skin changes (eg, dermatitis, edema, ulceration, etc. )
Treating varicose veins without surgery is a top priority. Potentially effective treatments for varicose veins include:
- Sclerotherapy. The introduction of a special drug into the vein, which leads to the gluing of the vessel walls
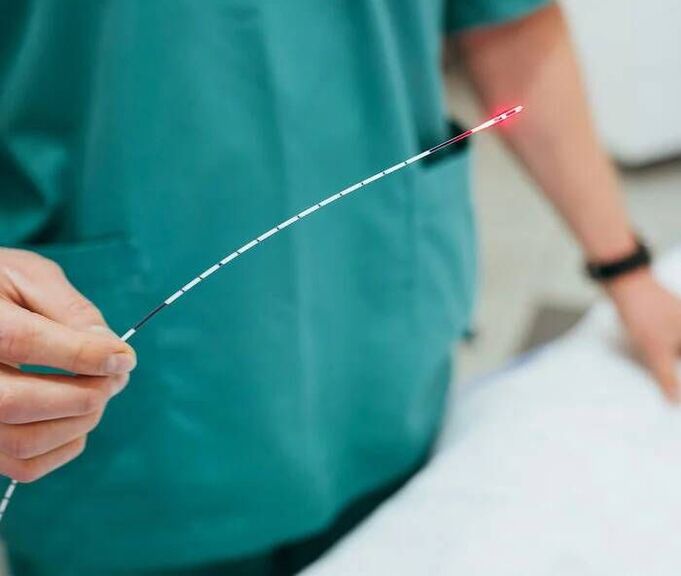
- Laser ablation Destruction of abnormal veins by radiofrequency, laser or other techniques
- Miniflebectomy. Painless surgical treatment of varicose veins


Is it safe to cure varicose veins?
On the Internet, you can often see search queries such as "varicose vein treatment drugs, varicose ointment treatment, varicose vein treatment at home, or varicose vein treatment with folk remedies. "Such methods lack an effective evidence base, and self-treatment only delays high-quality therapy and aggravates the condition of the veins.
Treatment of varicose veins with a laser is safe and affordable. The advent of minimally invasive therapy in the early 2000s led to a very favorable prognosis and minimal risks for most treatments.
It is important to contact a specialized phlebologist so that he can select an individual treatment plan that will focus on the specific course of your disease.
How to diagnose varicose veins?
- Physical examination. A phlebologist performs a physical exam and takes a complete medical history, taking into account the symptoms and condition of the venous system.
- Ultrasound examination. To detect venous insufficiency, the doctor will prescribe an ultrasound. A venous ultrasound allows for a complete evaluation of the venous system. Your doctor will check if you have blood clots by looking at the level of the varicose veins.


What happens if varicose veins are not treated?
If you don't feel any symptoms, you can check the condition of the veins without treatment. However, in some cases, varicose veins can lead to the development of blood clots or venous ulcers (wounds that don't heal). Sometimes a varicose vein can rupture and cause severe bleeding. If you have developed varicose veins, a consultation and examination by a phlebologist is recommended.



















